Bipartisan Effort Paves Way for Reviving Shuttered Hospitals in Georgia

In front of the closed Atlanta Medical Center, a message of ‘Stronger Together’ is painted next to a splash of summer hyacinth hydrangeas. It was relatively calm in the campus on a recent weekend because nearly two years ago, AMC shut down. There was a security car parked right behind the barbed wired fence; people walked past the scene unmindful of what was going on.
Down in Cuthbert, about 160 miles away, the Southwest Georgia Regional Medical Center is still closed after it was shut down four years back, another southern hospital that became a statistic in the area replete with them. ‘Even if a facility of a considerably lesser size was to replace the former Cuthbert hospital’ Whatley remarked, ‘the effect it would generate for the county would be tremendous’ –Steve Whatley, chair of the Randolph County Hospital Authority.
The two pilots included one inner-city hospital and the other, a rural health facility, and realized that, among other things they lacked sufficient patients with private health insurance.
This year, they also became the focus of attention for some of Georgia’s main legislative initiators. April saw Gov. Brian Kemp, the Republican, sign the legislation that had a clause sponsored by Democrat U. S. Sen. Jon Ossoff.
It changes the state’s procedure for granting “certificates of need” that enables existing hospitals and other health facilities to prevent rivals from expanding by showing that there is no demand for their services.
Certificate of need is practiced in 35 states and Washington D. C. as reported by the National Conference of State Legislatures. Most of the hospitals, particularly nonprofit ones, back the regulations and have said they lower the price of the health-care services and maintain high quality of medical care. Despite the fact that CON requirements are designed to protect patient’s interests, health providers are required to seek certain permissions in the state before adding some new services or before constructing new or expanding existing facilities.
Whether the laws enhance the quality of care or decrease costs is still open to question actuality opponents argue that a further introduction of competition will lower the expenditures of insurers and consumers. As far as the extension of CON programs is concerned, in 2018 the Trump administration issued a report suggesting states should repeal or modify CON requirements that they claimed drive up the price of the health care services.
“The case against CON laws is just too compelling: it gives a powerful message that these laws do not in fact reach for the intrinsically expressed aims of raising the availability, reducing costs, and enhancing the quality of the health services”.
Dan Sullivan, a Georgia based consultant who frequently works with hospitals and other medical facilities in their battle to retain the laws, stated that by restricting the quantity of suppliers who extend highly specialized health services like transplantation of vital organs, states can more appropriately perpetuate quality care.
But, certificate of need laws can cut health care fraud, said Sullivan. Indeed, many legal reforms in health policy in Florida also occurred after the Trump administration suggestion, including the repeal of the certificate of need for many health facilities, including hospitals. Mr. Bisht emphasised that fraud escalated in the state after regulations wallooned out.
That is why, for instance, at least when you file a CON, there is, at the very least, a semblance of investigation, according to Sullivan.
He stated it another advantage of the laws in that they often provide for minimum charity care requirements to be met.
Other Southern states have in recent years relaxed their certificate of need regulations. This year, Tennessee’s legislature okayed a bill that expands the list of professions that don’t have to apply for a certificate. North Carolina, for example, eased some restrictions in a reform that opened the door to Medicaid expansion last year. There was a major amendment of rules by South Carolina the previous year.
This year, Republicans in Georgia’s legislature sought to repeal the state’s certificate of need rules. It failed to achieve the goal because of stiff opposition from various hospitals.
Narrower legislation that Kemp signed would rather liberalise the guidelines for construction of rural hospitals and the bill does not apply to a possible new facility that Morehouse School of Medicine, one of the ubiquitously scarce historically black medical schools could possibly enter a partnership with.
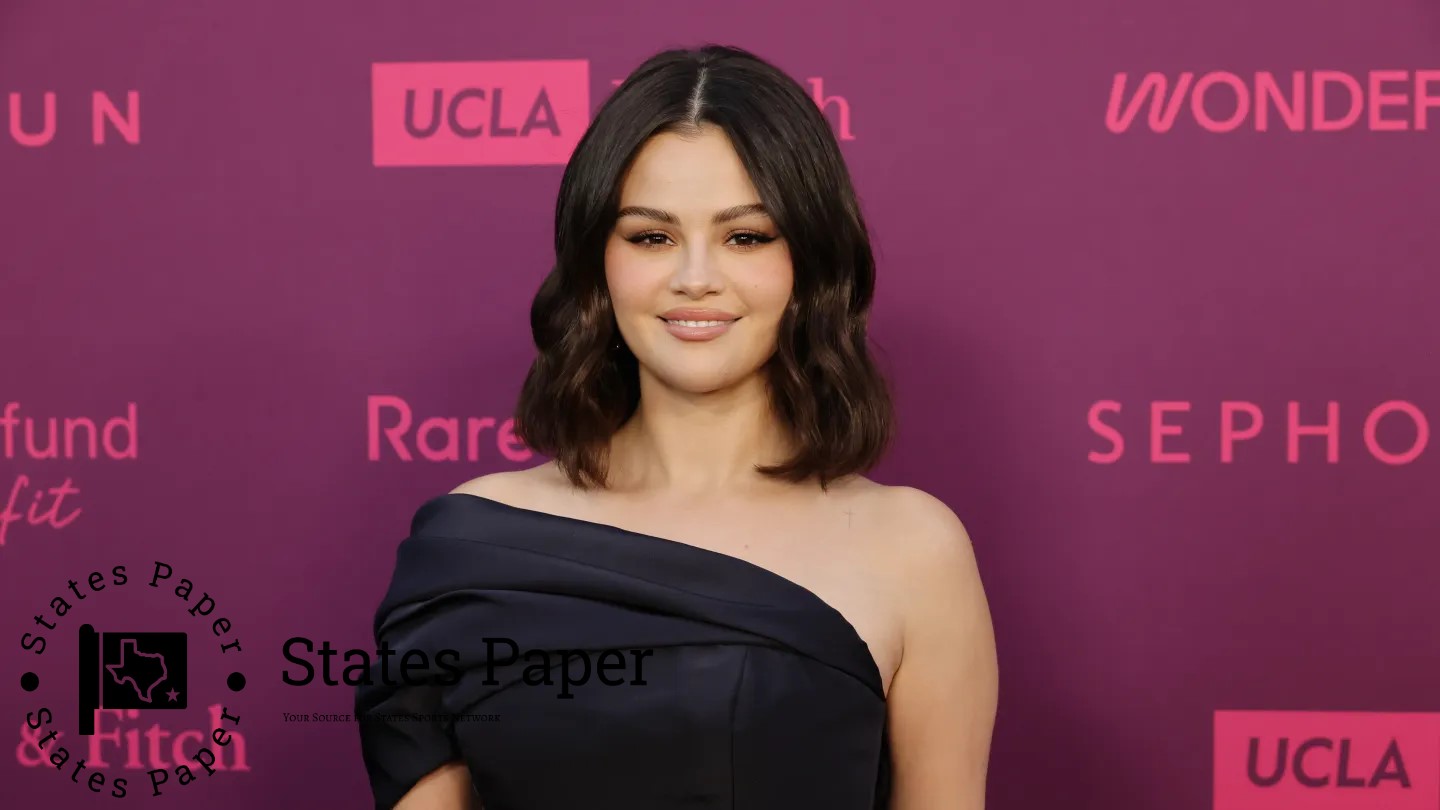
That could potentially fill much of the gap left by Atlanta Medical Center’s closing.
industry insiders opined that Morehouse might have to partner with a deep pocket and that Atrium Health which is part of Charlotte North Carolina based health system, Advocate Health may be a good fit. The mission focused, growth oriented nonprofit health system operates a clinic in association with Morehouse Healthcare in East Point, a suburb of Atlanta and is expanding in the state. Neither Morehouse nor Atrium responded to questions about a possible hospital partnership with KFF Health News.
The shuttered AMC main campus, on the other hand, remains locked in a moratorium the city placed on redeveloping the land — an action Wellstar Health System took to shock its stakeholders when it closed the hospital.
In 2022 the current Mayor of Atlanta, Andre Dickens signed an executive order pausing all development on the site indefinitely. He has also described the shutdown of one of Atlanta’s most crucial medical facilities as ‘abnormally hurried’.
Atlanta’s city council later on in June added another 120 days on the ban.
But building a new inner-city hospital “would be a heavy lift financially,” said Josh Berlin, the CEO of rule of three, an Atlanta-based health care consulting firm. That has been so because it would largely enlist from the area’s high proportion of the uninsured and Medicaid patients. Georgia is one among the 10 states which have not extended the Medicaid to full capacity, and so has a high proportion of its population that lack health insurance.
“You have a community, especially the elderly, which is yet to find where to seek care given the recent shutdown of Atlanta Medical Center,” he said.
It is also worth to note that other facilities in Atlanta including Grady Memorial Hospital has been receiving more patients after the shut down of AMC. One of the state dashboards frequently has statistics that define Grady as a ‘dangerously overcrowded’ hospital.
The volumes have increased the need to accommodate more patients pushing up the ratification of expansion goals for Grady that include more than 150 beds according to its chief strategy officer Shannon Sale. “We knew that was going to be needed over time. The Atlanta Medical Center closure sped up that process,” she said.
A lot less elaborate is the situation in southwestern Georgia.
Apparently, Whatley and other community leaders are waiting for the completion of a feasibility study which, in its turn, is expected to present the concept of a ‘rural emergency hospital’ – a new federal category that provides additional funding to facilities meeting its requirements.
It promised that extra Medicare payments would be made for hospitals in rural areas of a community and another payment of approximately $3. 2 million a year if they shut expensive inpatient offerings and exist as emergency and outpatient centers only.
Ossoff secured nearly $12m in three different appropriation’s bills for a rural emergency hospital in Cuthbert. He said he personally went to lobby with leaders of the state in order topen up the provision contained in the Georgia certificate of need bill. If it were to seek the status of rural emergency hospital, Southwest Georgia Regional Medical Center would have to obtain permission from the Federal Government because of its date of closure.
“This is a very challenging thing to do, and we’ve still got significant hurdles to clear,” at the KFF Health News Ossof said.
Even if the Cuthbert facility is reopened, it is going to be confronted with the same challenges that forced its closure in the first place – what Ossoff referred to as “failures of state policy. ” He was specifically referring to Georgia’s failure to expand the Medicaid program after the shutdown.
Brenda Clark who works in a wellness center across the street from the closed Cuthbert hospital said some of the people in the community do not believe the hospital will reopen again.
“It’s much needed”, she said, “People are hoping and praying we get it back. ” However, there are certain individuals, who can aptly term their statement as, ‘I will only believe when I have it in my sight whatsoever it may be. ’
 Asif Reporter
Asif Reporter